Plenaries, Presentations, Workshop Summaries & Slides
Day 1
Opening Plenary- Embracing Indigenous Wisdom on Holistic Wellbeing
Access Presentation SlidesModerator:
- Dr. Kate Mulligan (She/Her) Senior Director, Canadian Institute for Social Prescribing, Canadian Red Cross
Speaker:
- Elder Dr. Albert Marshall
Session Summary
How often do we make decisions with the next seven generations in mind? This profound question, posed during the opening plenary, invites us to reflect on the implications for policy, practice, and research—areas often focused on short-term outcomes rather than the long-term human wellbeing. Elder Dr. Albert Marshall offered critical insight, reminding us that while technology has brought many advances, it has also distanced us from our spiritual well-being and sense of interconnectedness.
“We’ve not just lost connection to the natural world, we’ve also lost connection with each other," Elder Marshall emphasized. "We have disconnected ourselves from the very essence of life and fallen for the false sense of security that science will somehow save us from all things”. His words call for a shift in our collective approach. The real challenge and opportunity lie in whether we can work together, humbling ourselves for the benefit of all, recognizing that the teachings of today will bring gifts that endure far beyond our lifetimes.
This reflection resonates with the principles of social prescribing, which seek to restore connections, both to our communities and to nature. By fostering a holistic approach to health and wellbeing, social prescribing is an act of care for the present and future, ensuring that we nurture ourselves and the generations to come.
Using The Healthy Aging Asset Index to Support Shared Social Prescribing Decision Making with Older Adults
Access Presentation SlidesSpeakers:
- Beth Mansell (She/Her) Provincial Social Prescribing Project Manager, Healthy Aging Alberta
- Colleen Derksen (She/Her) Social Work Manager, Sage Seniors Association
- Dr. Tammy O'Rourke (She/Her) Associate Professor, Athabasca University
Session Summary
“Meeting seniors where they are” was the core theme of this session. Funded by the Canadian Frailty Network and Max Bell Foundation, and developed with partners from the University of Alberta and Athabasca University, the HAAI tool empowers older adults by facilitating personalized health assessments across domains such as physical health, social engagement, and personal well-being. HAAI aims to enable older adults to set and pursue their own goals while integrating support from professionals, community organizations, and volunteers.
Speakers highlighted promising data showing significant improvements in personal well-being and social engagement for seniors after six to twelve months of HAAI-guided social prescribing, with many reporting reduced isolation and better social connections. Key calls to action included expanding the HAAI tool across more community agencies and health services to amplify its benefits. As one participant noted, “building rapport” is essential, allowing seniors to engage fully with the process. Through HAAI, social prescribing can be further tailored to Canada’s aging population, fostering a more inclusive and responsive approach to care.
Building Trust and Collaboration: Equity and Core Principles of Social Prescribing
Access Presentation SlidesModerator:
- Dr. Alayne Adams (She/Her) Professor, McGill University
Speakers:
- Le-Tien Bhaskar (She/Her) Co-Founder and Co-Lead, Canadian Social Prescribing Student Collective
- Dr. Kiffer Card (He/Him) Assistant Professor, Simon Fraser University
- Caitlin Muhl (She/Her) PhD Candidate in Health Quality, Queen's University
Session Summary
In exploring trust within social prescribing, Prof. Kiffer G. Card, Caitlin Muhl, and Le-Tien Bhaskar delved into the complexities of fostering social wellbeing, particularly among older adults. As we age, our social networks often shrink, prioritizing fewer but deeper relationships. Social prescribing seeks to address isolation, but promoting belonging can sometimes challenge an individual's sense of autonomy. Trust becomes a crucial yet complicated factor in this dynamic, with patients often feeling that their prescribers don’t fully understand their personal contexts. Le-Tien captured this challenge, highlighting that “there is a disconnect between the extent of co-production and between policy and practice.” Prof. Card further asked, "How can we build trust when health providers can't practically forge genuine psychological connections with every patient?"
A key takeaway was the importance of empowering individuals rather than making assumptions. Trust, as Prof. Card emphasized, starts when people feel seen, respected, and understood. “The way we’ve structured our healthcare system is antithetical to building trust,” he added. The session called for balancing autonomy and belonging, ensuring culturally sensitive, personalized care, and co-producing solutions that recognize patients' needs.
Black Social Prescribing for Black Health
Access Presentation SlidesModerator:
- Kisa Hamilton (She/Her) Co-founder/Consultant, Transform Practice Co-operative Inc
Speakers:
- Hathor-Ra Phoenix Adwoa (She/Her) Black Focused Social Prescribing Navigator, TAIBU Community Health Centre
- Joesiann Nelson (She/Her) Director of Health Promotion and Community Services, Black Creek Community Health Centre
- Neil Price (He/Him) Executive Director, Logical Outcomes
Session Summary
This session emphasized the need for tailored, community-driven approaches in addressing health inequities within Black communities, that are deeply rooted in community knowledge and cultural safety. "We can do social prescribing, but it has to be through a Black-focused lens in this community," stated Joesiann Nelson, emphasizing the importance of culturally specific programming. Afro-centric principles and participatory evaluation approaches and continuous community involvement were identified as essential to designing effective, culturally safe social prescriptions.
Evaluation processes grounded in anti-racist principles were highlighted as critical, requiring trust, flexibility, and time to fully reflect community needs and values. This slower, deliberate process was seen as essential for fostering meaningful, long-lasting impact. Neil Price in presenting the BFSP project evaluation results, highlighted the vital role of food security, with 60% of survey respondents accessing food programs through BFSP. The session stressed that access to food and housing, among other basic needs, precludes other social prescriptions. "There are social determinants of health and there are social determinants of equity" said Hathor-Ra, reflecting on the necessity of meeting basic needs before implementing other interventions.
The session called for long-term, sustainable funding tailored to Black community needs, advocating for core funding rather than project-based approaches as Joessian Nelson urged. "We are not projects; we are human beings”.
Holding and Discretion as Part of The Link Worker Role: Building on Findings from A Multi-Site Study Conducted in England
Access Presentation SlidesSpeakers:
- Debra Westlake (She/Her) Research Fellow, University of Oxford
- Stephanie Tierney (She/Her) Associate Professor, University of Oxford
Session Summary
In this session, Debra Westlake and Stephanie Tierney examined the complex role of Link Workers (LWs) within the healthcare system, focusing on both challenges and critical concepts that shape their impact. Key issues include the variability in time available for client interactions, challenges to role credibility when LWs work part-time or across multiple practices, and limited involvement in multidisciplinary teams. Westlake and Tierney highlighted the delicate balance required between the quantity and quality of client encounters, emphasizing that the concepts of "holding" and "discretion" are central to quality interactions and effective relationship-building.
The concept of “holding” emerged as a cornerstone of impactful client interactions. More than active listening, “holding” involves creating a secure, emotionally supportive space where clients feel empowered to express themselves. A social prescribing connector in the session shared that “holding” allows them to “Do with people rather than for people...sometimes somebody needs that extra something to get them over that hump”. This approach enables LWs to support clients through emotional distress and help them prepare for change. However, “holding” can affect the emotional well-being of LWs themselves, underscoring the need for targeted training and support.
The second concept, “discretion,” refers to the judgment required to balance institutional policies with individual client needs. Discretion allows LWs to personalize their approach, but unstructured discretion can create risks without adequate training. As one participant noted, "some discretion should be there, and we should be able to bring that forward to funders and organizations," emphasizing the need for flexibility and support in the LW role.
Supporting Caregivers: Innovations in Social Prescribing Programs Across Canada
Access Presentation SlidesModerator:
- Liv Mendelsohn (She/Her) Executive Director, Canadian Centre for Caregiving Excellence
Speakers:
- Adrien McKenna (She/Her) Caregiver Link Worker, The Ontario Caregiver Organization
- Felicia Hart (She/Her) Manager, Caregiver Navigation and Workplace Programs, The Ontario Caregiver Organization
- Barb MacLean (She/Her) Executive Director, Family Caregivers of BC
- Wendy Johnstone (She/Her) Director of Programs & Innovation, Family Caregivers of BC
- Aaron Yukich (He/Him) Project Lead, Caregiver Rx Social Prescribing Program, Family Caregivers of BC
Session Summary
The session on social prescribing for caregivers highlighted its emerging role in addressing the complex challenges faced by this often-overlooked group. With one in four Canadians currently serving as caregivers—and one in two expected to take on this role in their lifetime—the need for comprehensive support is critical. Key insights reveal that nearly half of Canadian caregivers report fatigue, over a third feel overwhelmed, and 80% express a desire for more social support, emphasizing the urgency of intervention. As noted during the session “Caregiving is a gift. It's something we do out of relation and relationships,” highlighting the relational aspect of caregiving in community building.
The call to action is clear: healthcare providers must lead the charge in identifying and supporting caregivers, with 77% of them wishing for inquiries about their own health during appointments. Implementing tailored social prescribing pathways can bridge the gap between healthcare and community support, necessitating collaboration among healthcare providers, community organizations, and caregivers themselves. The session emphasized that caregivers are integral to the health and social care teams; their systematic involvement in social prescribing approaches is the next frontier for creating effective and integrated support systems.
Braiding Knowledges, Theory, and Practices: Indigenous Determinants of Health and Social Prescribing in Canada
Access Presentation SlidesModerator:
- Jean-Philippe Crete (He/Him) Director of Research & Policy - Office of Indigenous Relations, Canadian Red Cross
Speakers:
- Jennifer Bull, Regional Action Plan Project Manager - Tuberculosis Elimination File, Nunatsiavut Government
- Kristen Jordan (She/Her) Public Health Advisor, Canadian Red Cross
Session Summary
The session focused on reframing medicine to prioritize wellness by recognizing the crucial role of community support which is often overlooked in mainstream healthcare. A key insight shared was that for Indigenous communities, wellness involves restoring broken relationships with each other and with the land. This perspective highlights the need for a more integrated approach, acknowledging that trust is foundational to effective healthcare: "People don’t care if they don’t trust," as noted by Jennifer Bull.
Cases and stories presented underscored the importance of tailored treatment plans, such as incorporating culturally appropriate, familiar foods into dietary recommendations, which can significantly enhance patient engagement and satisfaction. The session emphasized that a wrap-around approach is essential to enact meaningful changes in health outcomes. As Kristen Jordan eloquently stated, "Just you, all by yourself, can help." Healthcare and community service providers are called to start from where patients are, understanding their unique contexts before proposing solutions. The session reinforced the need for a holistic view of health that connects individuals to their communities and environments, ultimately driving more effective healthcare practices.
Revolutionizing Food Accessibility: Integrating Dignity-Centered Approaches in Fresh Food Prescribing Programs
Access Presentation SlidesModerator:
- Albesa Aliu (She/Her) PhD Candidate, University of Montreal
Speakers:
- Beccah Frasier (They/She) Executive Co-director, Carrefour Solidaire CFC
- Lizzie Slattery (She/Her) Mobilization + Engagement Coordinator, Carrefour Solidaire CFC
- Matthew Little (He/Him) Assistant Professor, School of Public Health and Social Policy, University of Victoria
Session Summary
Researchers Beccah Frasier and Lizzie Slattery from Carrefore Solidaire shared the significant reach of the Community Food Centre which has supported 1,553 households and 4,166 individuals $565,500 in support, with a 93% usage rate in 2023. The program operates through a network of 44 community organizations distributing Carrefour Points (CP) and 54 partner markets accepting CP. Initially a seasonal program, it became an annual initiative in 2022 and is gearing up for expansion in three neighborhoods for 2024-2025. A standout feature of the Carrefour food security program is its community-driven, tech-forward, and flexible approach that is tailored to specific neighborhoods, increasing access to food resources and fostering a sense of community.
Matthew Little of Guelph CHC shared the reach of the Fresh Food Rx Program, which has provided food prescriptions to address food insecurity and nutrition-related health outcomes. In 2021-2022, 60 participants received dietitian support, recipe ideas, and vouchers for fruits and vegetables. With an 88% voucher redemption rate, participants accessed an average of $1,340 worth of produce. Fruit and vegetable consumption increased, especially among those most food insecure.
Both programs emphasize empowerment, as one speaker shared “Trust people to make their own choices in the things they need." The researchers emphasized the urgent need for a structured, policy-level solution addressing income insecurity, as “food insecurity is fundamentally a problem of inadequate income, not a lack of food”. Addressing income inequality is critical to lasting food security solutions.
How to Harness the Power of Students to Support the Canadian Social Prescribing Movement
Access Presentation SlidesModerator:
- Benji Finestone (He/Him) Events Lead, Canadian Social Prescribing Student Collective
Speakers:
- Jeffrey Wong (He/Him) Local Initiatives Co-Lead, Canadian Social Prescribing Student Collective
- Le-Tien Bhaskar (She/Her) Co-Founder and Co-Lead, Canadian Social Prescribing Student Collective
- Margaret Lin (She/Her) Social Prescribing Change Lead, Fraser Health Authority
- Nina Doad, Co-Lead, Canadian Social Prescribing Student Collective
- Tarek Hussein (He/Him) PharmD for Pharmacists Student, The Lesley Dan Faculty of Pharmacy, University of Toronto
Session Summary
This session spotlighted the enthusiasm and potential of students as champions of social prescribing, both on and off-campus. Students shared a strong belief in the power of social prescribing to address post-pandemic issues of isolation and loneliness, noting its potential to foster community and support mental health on campuses. Speakers emphasized the need for social prescribing education beyond medical schools, suggesting it be integrated into other health and allied health fields to broaden its impact.
School administrators voiced an interest in social prescribing for its potential to improve student retention but expressed a need for case studies and proven frameworks before committing resources. Notably, two college administrators discussed the challenge of initiating social prescribing on campuses and underscored the importance of student-led initiatives. A memorable quote capturing the student perspective was: “Social prescribing belongs on campus—our peers need it now more than ever.” The session called for increased student support in driving these efforts and underscored the importance of collaboration between educational institutions and the social prescribing movement.
Integrating Green Spaces, Nature, and Arts for Community Health and Equity
Access Presentation SlidesModerator:
- Laura Isidean (She/Her) Advisor, Canadian Red Cross
Speakers:
- Dr. Carolyne Clare (She/Her) Research Fellow, BC Alliance for Arts and Culture
- Joy Sammy (She/Her) Manager Research and Partnerships, Park People
- Dr. Samantha Evans, Founder and Managing Director, Cultivating Community, UK
- Susanna Fong (She/Her) Administrative Coordinator, BC Alliance for Arts + Culture
Session Summary
There is a transformative potential for public spaces like city parks in addressing urban challenges like mental health and social isolation. Key takeaways highlighted the essential role of park-based organizations, often volunteer-run, as crucial assets in the social prescribing ecosystem. Notably, 80% of city residents report positive mental health impacts from parks, with involvement in park stewardship activities, such as tree planting, significantly enhancing happiness and connection to nature.
The discussion also pointed to the need for equity and accessibility in green social prescribing, particularly in identifying underserved groups and improving access to nature. Speakers urged a shift from patient-only care to include caregivers, recognizing that 20% of caregivers are seniors themselves and often "one fall away from not being able to provide care." The call to action included integrating park organizations more effectively with prescribers, developing standardized guidelines for nature-based interventions, and fostering cross-sector collaboration between health sectors and park organizations. As one speaker poignantly noted, “One small connection can lead to incredible change,” underscoring the session's alignment with the conference's focus on community-centered healthcare approaches. By integrating urban green spaces into social prescribing, we can reimagine parks as vital hubs for well-being and equity, ultimately enhancing the narrative of social prescribing in addressing complex urban health challenges.
Storytelling As a Method of Surfacing the Experiences of Older People from Ethnically Minoritized Communities Engaging in Cultural Social Prescribing Activities: The TOUS Study
Access Presentation SlidesModerator:
- Shereen Zahid (She/Her) Communications and Knowledge Mobilization Specialist, The Canadian Institute for Social Prescribing
Speakers:
- Debra Westlake (She/Her) Research Fellow, University of Oxford
- Stephanie Tierney (She/Her) Associate Professor, University of Oxford
Session Summary
The presentation highlights storytelling as a valuable research tool in social prescribing, offering richer, more nuanced data compared to traditional methods. It underscores the multifaceted role of the cultural sector in social prescribing, which includes providing therapeutic spaces, immersive activities, and opportunities for social connection. Tailored and empathetic messaging is crucial for effective engagement in cultural programs, and these initiatives should be viewed as part of a broader movement toward addressing intersecting barriers to well-being.
Key insights reveal that cultural activities can develop social capital—both internal (trust) and external (practical support) —and that therapeutic landscapes in cultural settings significantly contribute to holistic well-being.
To enhance the effectiveness of social prescribing, there are several key actions to consider. First, increasing collaboration between health professionals and cultural providers is essential for integrating therapeutic landscapes into care pathways. Additionally, expanding the use of storytelling as an evaluation tool in social prescribing research can provide deeper insights. Developing personalized and empathetic messaging strategies will improve engagement in cultural programs, while designing interventions that address multiple, intersecting barriers to well-being is vital. Finally, tailoring cultural activities to be more accessible, relevant, and inviting—especially for older adults—can play a transformative role in enhancing overall well-being.
Plenary Panel - Global Perspectives on Social Prescribing
Access Presentation SlidesModerator:
- Dr. Kate Mulligan (She/Her) Senior Director, Canadian Institute for Social Prescribing, Canadian Red Cross
Speakers:
- Dr. Alan Siegel (He/Him) Co-founder, Social Prescribing USA
- Charlotte Osborn-Forde (She/Her) Chief Executive Officer, National Academy for Social Prescribing
- Dr. J R Baker (He/Him) Chair, Australian Social Prescribing Institute of Research and Education
- Prof. Kheng Hock Lee (He/Him) Associate Professor, SingHealth Community Hospitals
- Dr. Thiago Trindade (He/Him) Assistant Professor, Federal University of Rio Grande do Norte, Brazil
Session Summary
The session emphasized the critical role of community involvement in the success of SP programs worldwide. Regardless of country or system, participants agreed that the community and voluntary sectors are essential partners in meeting the health and social needs of individuals. “You can have a medical model and an alternative community model, and the beauty is in bringing them together,” said Charlotte Osborn-Forde, emphasizing SP's potential to bridge these sectors and improve overall well-being.
Country-specific insights highlighted the diversity in SP implementation. In England, social prescribing link workers (SPLWs) have become mainstream, with over 3,500 workers in GP practices and millions of referrals. Meanwhile, Australia and Brazil have seen grassroots and private sector initiatives integrate SP with national health systems, while Singapore's approach evolved from hospital-centered care to community integration to address the fragmentation of care. As Dr. Thiago Trindade from Brazil noted, "We need to create a network...we won’t solve problems by giving more pills."
The session also highlighted significant challenges, particularly around funding for the voluntary sector and the need for cross-governmental approaches. There was a strong call for expanding SP beyond healthcare into sectors like employment and social welfare, as Osborn-Forde remarked “Social prescribing has been tested in primary care, and now it is time to expand to other sectors”.
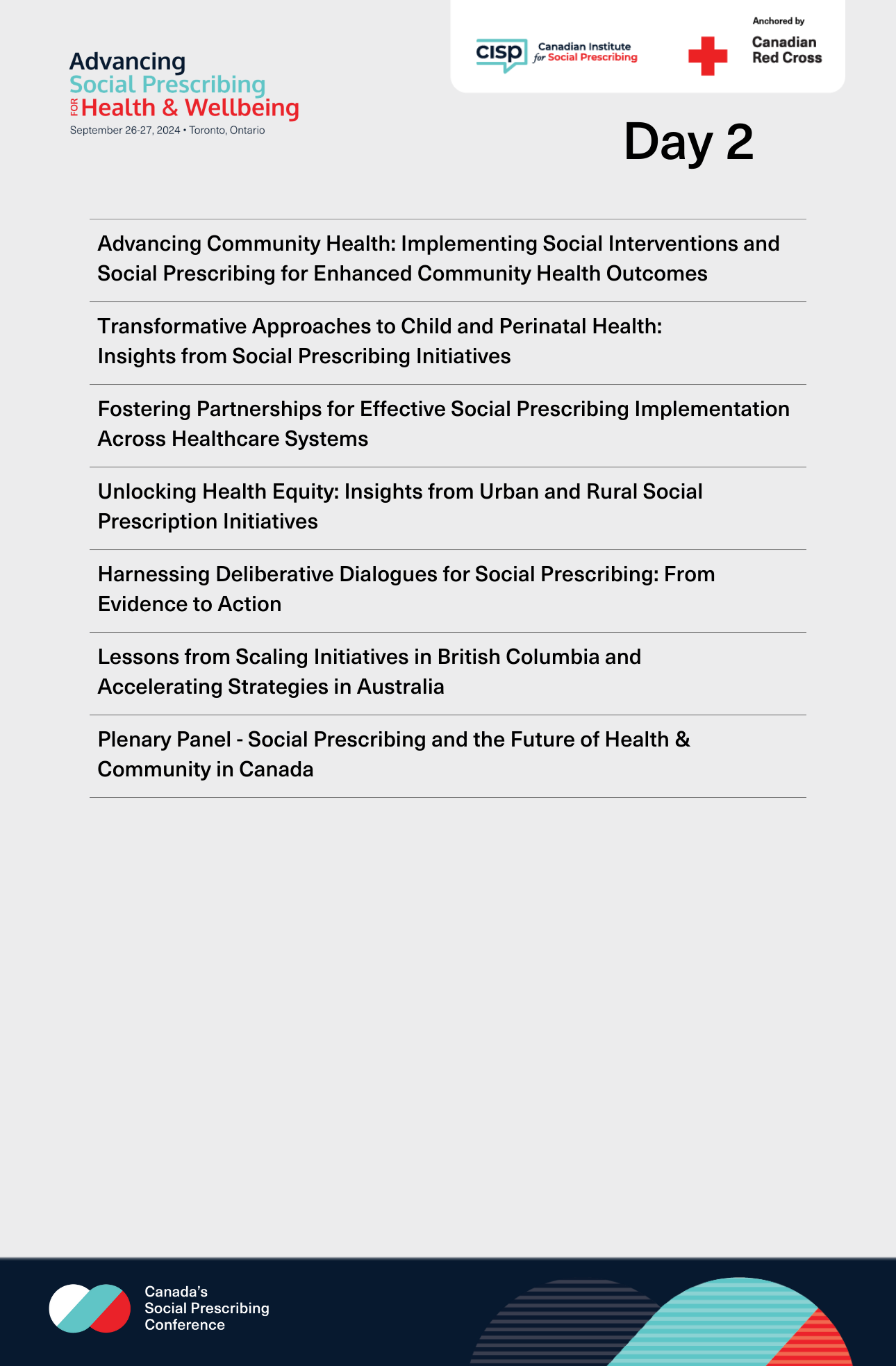
Day 2
Advancing Community Health: Implementing Social Interventions and Social Prescribing for Enhanced Community Health Outcomes
Access Presentation SlidesModerator:
- Natasha Beaudin (She/Her) Social Prescribing Project Lead, Alliance for Healthier Communities
Speakers:
- Dr. Gary Bloch (He/Him) Physician Lead, Social Interventions and Equity, St. Michael's Hospital Academic Family Health Team
- Jayne Nelson (She/Her) Chief Executive Officer, IPC Health
- Maria Hussey (She/Her) Wellbeing Coordinator, IPC Health
- Nassim Vahidi-Williams, Manager, Patient and Community Engagement, Unity Health
- Orit Adose (She/Her) Community Health Worker, St. Michael's Hospital Academic Family Health Team
- Sandesh Basnet (He/Him) Social Prescribing Link Worker, St. Michael's Hospital Academic Family Health Team
Session Summary
This session featured inspiring stories and examples of community partnership, individual empowerment and holistic care that seeks to address the social determinants of health. Jayne Nelson and Maria Hussey of IPC Health (a model in which clinicians act as wellbeing coordinators to facilitate warm referrals for social support) shared a story of a client experiencing homelessness, who after receiving support from IPC Health, transitioned into volunteering as a peer support worker. Dr. Gary Bloch and Nassim Vahidi Williams of St. Michael’s Hospital Academic Family Health Team described a powerful initiative which began with the identification of a need for cleaning services among older adults. The team responded to this need by partnering with a local community leader who provides cleaning services- “We identify the community needs and empower a service within the community to meet that need”. Speakers expressed that by building partnerships with community-based organizations, health systems can expand their reach and improve service accessibility, ultimately benefiting individuals and communities.
Dr. Bloch emphasized the need for health equity-focused data collection that captures community health determinants such as income levels and language barriers – “Capturing this data allows us to think about how we design social prescribing services, with this type of understanding of our community in mind.” To revolutionize primary care, the session called for the extension of this model throughout the broader healthcare system which requires outreach, education, and a willingness to confront the gaps in care. “Culture change takes years,” the speakers acknowledged, but they affirmed that progress is being made, illustrating that social prescribing is not only necessary but also achievable within traditional healthcare frameworks.
Transformative Approaches to Child and Perinatal Health: Insights from Social Prescribing Initiatives
Access Presentation SlidesModerator:
- Le-Tien Bhaskar (She/Her) Co-Founder and Co-Lead, Canadian Social Prescribing Student Collective
Speakers:
- Beth Tupala (She/Her) RN, Project Manager and Clinical Navigator, Ask Masi Project, The Ottawa Hospital, Carleton University
- Caitlin Muhl (She/Her) PhD Candidate in Health Quality, Queen's University
- Dr. Sue Bennett (She/Her) Pediatrician and Director Social Pediatrics, CHEO, Professor Pediatrics, uOttawa
Session Summary
The session showcased two innovative programs promoting mental health through social interventions, particularly focusing on early intervention strategies. The first program, the inaugural social prescribing initiative for children and youth in Canada, takes place in an underserved neighborhood in Ottawa. By collaborating with a connector, children engage in co-designing their social prescriptions, which encompass non-medical activities tailored to their interests, such as visiting fire stations or going to camp in nature. This initiative underscores the importance of "meeting the family and kids where they are," as emphasized by Caitlin Muhl, and aims to foster connections to their communities, that will pave the way for improved health and wellbeing.
The second program, Ask Masi, addresses the critical intersection of parental mental health and early childhood development. Recognizing that many pregnant and postpartum individuals experience anxiety and low mood, Ask Masi equips healthcare providers with tools to recommend community-level interventions instead of unnecessary psychiatric referrals. The program emphasizes the integration of social and medical models of health, with a focus on perinatal mental health navigation to enhance patient support. By understanding the unique needs of children and their families, and recognizing the social determinants of health, attendees left inspired to advocate for innovative, community-based solutions in mental health care.
Fostering Partnerships for Successful Social Prescribing Implementation Across Healthcare and Social Systems
Access Presentation SlidesModerator:
- Bobbi Symes (She/Her) Director, Healthy Aging, United Way British Columbia
Speakers:
- Dr. Alayne Adams (She/Her) Professor, McGill University
- Catherine Paquet, Associate professor, Université Laval
- Dr. Grace Park (She/Her) Regional Medical Director, Fraser Health Authority
- Madison Legatt (She/Her) MSc, McGill University
- Margaret Lin (She/Her) Social Prescribing Change Lead, Fraser Health Authority
- Paola Leal (She/Her) Director, Community and Knowledge Development, Eva Marsden Centre for Social Justice and Aging
Session Summary
This session on effective implementation of social prescribing explored how a strategic, multi-faceted approach can transform community health. The discussion highlighted the vital role of community engagement, trust-building, and local partnerships in making social prescribing a success. Central to this effort are community-based link workers and the active involvement of healthcare providers, particularly primary care physicians, who help ensure that engagement methods are inclusive and accessible to all.
As the conversation unfolded, it became clear that the implementation process is complex. Tensions arise when addressing basic needs like housing and food security alongside additional social prescriptions, especially in resource-limited settings. Participants emphasized the need for structured discussions with stakeholders to identify barriers and invest in link workers who can bridge the gap between healthcare and social services. One participant captured the essence of the experience, saying, “It's more than a method. It was a process, and a transformative experience for many.”
The session also showcased the distinct paths taken by British Columbia and Quebec in their social prescribing efforts. BC’s health policy-driven model integrates health and social care, offering a well-resourced framework for supporting healthy aging. In contrast, Quebec’s grassroots approach fosters localized innovation but adds layers of complexity as stakeholders navigate diverse needs. Together, these models illustrate the profound importance of addressing the social determinants of health and striving to reduce health inequities, ultimately paving the way for a more inclusive healthcare landscape.
Harnessing Deliberative Dialogues for Social Prescribing: From Evidence to Action
Access Presentation SlidesSpeakers:
- Catherine Paquet, Associate professor, Université Laval
- Dr. Alayne Adams (She/Her) Professor, McGill University
- Madison Legatt (She/Her) MSc, McGill University
- Nicole George (She/Her) PhD Candidate, McGill University
- Paola Leal (She/Her) Director, Community and Knowledge Development, Eva Marsden Centre for Social Justice and Aging
- Syrine Gamra (She/Her) MPH Candidate, McMaster University
Session Summary
Social prescribing is emerging as a transformative approach to healthcare, addressing the complex interplay between social determinants and health outcomes. Based on the discussion and data presented, there is a critical need for a holistic, collaborative approach to implementing social prescribing pathways. Key insights reveal that while technological solutions like universal assessment tools and electronic referral systems are beneficial, the core elements of successful social prescribing lie in human-centered aspects such as active listening skills, community engagement, and addressing fundamental needs like housing and food security.
The call to action is clear: healthcare providers, community organizations, and policymakers must collaborate to implement comprehensive social prescribing pathways. This includes prioritizing the training of link workers, fostering partnerships with community agencies, and ensuring that basic needs like housing and food security are addressed as part of the prescribing process. By focusing on these critical elements and utilizing techniques like deliberate dialogue to generate collective wisdom, we can create more effective, inclusive, and sustainable social prescribing initiatives that truly address the holistic needs of individuals and communities.
"Assume clients have equal voice; do not assume people speak the same language."
Unlocking Health Equity: Insights from Urban and Rural Social Prescription Initiatives
Access Presentation SlidesModerator:
- Beth Mansell (She/Her) Provincial Social Prescribing Project Manager, Healthy Aging Alberta
Speakers:
- Dena Silverberg (She/Her) Project Coordinator, Older Adult Centres’ Association of Ontario
- Dr. Megan MacGillivray (She/Her) Assistant Professor, St. Francis Xavier University
- Krista Mulbery (She/Her) Social Prescribing Project Manager, Edmonton Seniors Coordinating Council
- Natasha Beaudin (She/Her) Social Prescribing Project Lead, Alliance for Healthier Communities
- Kathleen Dolan, St. Francis Xavier University
Session Summary
This session brought together diverse perspectives from Alberta, Ontario, and Nova Scotia to explore the unique implementation of social prescribing in Canada, particularly its application to older adults and rural communities.
A central takeaway was the critical importance of fostering trust between service providers and clients. Whether through regular follow-ups or personalized supports, building one-on-one relationships enhances the success of social prescribing interventions. As noted by Dena Silverberg, “Anything that removes barriers to prescription, we have or we can add at the Seniors Active Living Centres (SALC), whether it’s transportation or special equipment.” This underscores how adaptable and community-driven social prescribing is, with the potential to meet specific needs in both rural and urban contexts.
Another key insight is that while funding plays a pivotal role in scaling these services and creating multi-disciplinary teams, the true driving force behind social prescribing is community, not healthcare alone. The session highlighted that with additional support and resources, barriers such as transportation and access to necessary equipment can be mitigated. Programs need to remain flexible and personalized to address the unique needs of populations, especially in rural areas.
Lessons from Scaling Initiatives in British Columbia and Accelerating Strategies in Australia
Access Presentation SlidesModerator:
- Dr. Kate Mulligan (She/Her) Senior Director, Canadian Institute for Social Prescribing, Canadian Red Cross
Speakers:
- Angela Sealy (She/Her) Community Connector, Parkgate Society
- Bobbi Symes (She/Her) Director, Healthy Aging, United Way British Columbia
- Dr. J R Baker (He/Him) Chair, Australian Social Prescribing Institute of Research and Education
- Leanne Wells (She/Her) Chair, Consumer and Community Expert Advisory Committee, Australian Social Prescribing Institute for Research and Education
Session Summary
The session highlighted the distinctive models and collaborative efforts driving social prescribing (SP) forward in different regions, with British Columbia (BC) and Australia (AU) offering key insights.
In BC, a unique, long-standing model was showcased, where trust has been cultivated through years of government funding for community-based social services (CBSS), particularly through the "Better at Home" program, which reaches communities across the province. This model has set a foundation for collaborative success. Reflecting on the value of collaboration, Angela Sealy a BC-based community connector stated, “As a scuba diver, you learn to collaborate, or you don’t come back.” Collaboration between senior organizations, peer support groups, and community organizations is well-established, with most referrals originating from Vancouver Health.
Australia's SP approach emphasized advocacy and coalition-building among influential stakeholders, including the College of General Practitioners, the National Health Foundation, and Diabetes AU. These groups collectively advocate for SP, sending a clear message to policymakers. “When organizations come together and say, ‘SP is a thing with a growing evidence base, we want to see it embedded in our system,’ governments generally listen.” This network effect has seen SP integrated into AU’s long-term preventive health plans. However, securing consistent funding remains a challenge despite these commitments.
Angela Sealy underscored the urgency of SP in the context of an aging population, describing it as the necessary intervention to manage the demographic shift: “The great tsunami [older adult population growing] is here, and SP is the sandbags to address this tsunami. Strengthening social capital one person or group of people at a time.”
Plenary Panel - Social Prescribing and the Future of Health & Community in Canada
Access Presentation SlidesModerator:
- Jodeme Goldhar (She/Her) Vice Chair Board of Directors, International Foundation for Integrated Care
Speakers:
- Dr. Jo Henderson (They/Them) Scientific Director - McCain Centre for Child, Youth and Family Mental Health, Centre for Addiction and Mental Health
- Kahir Lalji (He/Him) Provincial Director, Government Relations & Programs, United Way British Columbia
- Lynn Taylor (She/Her) Special Advisor, Health Transformation Executive Council, Gov NL
- Dr. Michael Routledge (He/Him) Medical Advisor, Manitoba Association of Senior Communities
Session Summary
In a forward-looking discussion, this session outlined a vision for Canada’s future health landscape, one where health, social, and community sectors are integrated and resourced to collaboratively enhance quality of life nationwide. Panelists, including notable speakers such as Jodeme Goldhar, underscored the transformative potential of social prescribing to address not just medical needs but the broader social determinants that impact health. Goldhar’s call to action, “Connection is the Correction,” resonated as a powerful reminder of the necessity of fostering connections across sectors to close gaps in care and support.
Speakers highlighted the critical need for cross-sector partnerships, emphasizing that meaningful change will require collaborative efforts to build a more connected and equitable system. They advocated for whole-person care and encouraged attendees to see their own roles in driving transformation within their communities. Participants were urged to champion a simpler, more accessible approach to health solutions, with several presenters showcasing successful, scalable models that demonstrate impact without complexity. This session left attendees with a call to rethink traditional structures, advocate for integrated care, and be catalysts in the movement for a healthier, more connected Canada.